1950-1957
Planting the seeds of lifelong passions
Although my life began in mid-20th century Chicago, my family’s Orthodox Jewish traditions were holdovers from their Eastern European roots. As a result, I attended kindergarten and 2nd grade in a parochial school, learning Hebrew in the mornings, and conventional English subjects in the afternoon. I think this photo was taken in the cloakroom at that school, and given the bowtie and cufflinks, I’m dressed up for some holiday.
I didn’t like this school and much preferred to think about cars. I studied the automobile dealer pages in the phone book until I had memorized every model. I was proud to be able to precisely identify the make, model, and year of almost any car on the road, just from seeing its taillight or bumper shape.
My parents also felt I needed music lessons. But why accordion? The only music studio close by? At any rate, I learned to read music and play some accordion standards. Any requests for Lady of Spain — anyone…anyone…anyone?
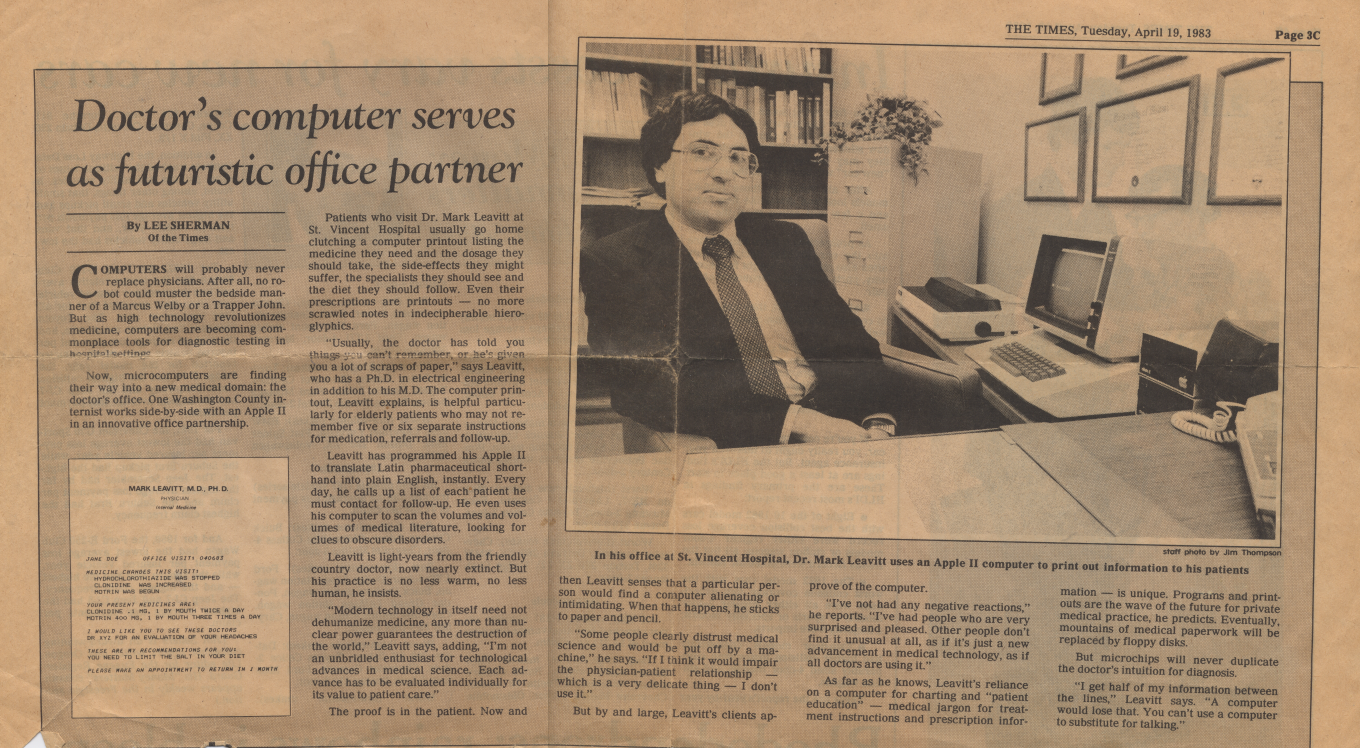
Following a rather traumatic hospitalization for asthma, I also became interested in doctors and medicine — I liked their white coats, stethoscopes, and the respect they commanded. Young boys were frequently asked what they wanted to be when they grew up, and I quickly learned that “doctor” was the correct answer to that question.
In 1957 our family moved to Tucson, Arizona, where the climate was believed to be more healthful for my asthma. There, these three seeds — cars, music, and medicine — would later sprout into lifelong passions.